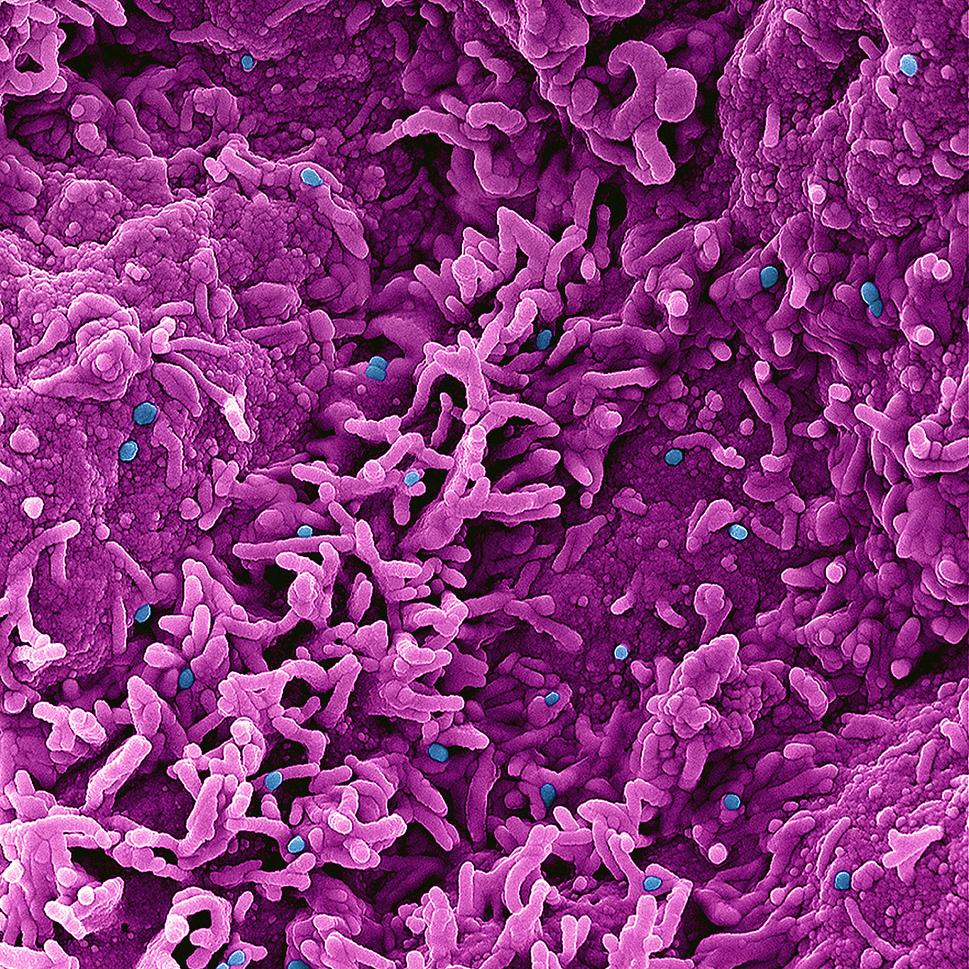
Colorized scanning electron micrograph of mpox virus particles (blue) on the surface of infected VERO E6 cells (pink). NIAID
A dose-sparing intradermal mpox vaccination regimen was safe and generated an antibody response equivalent to that induced by the standard regimen at six weeks (two weeks after the second dose), according to findings presented at the European Society of Clinical Microbiology and Infectious Diseases Global Congress in Barcelona.
The results suggest that antibody responses contributed to the effectiveness of dose-sparing mpox vaccine regimens used during the 2022 U.S. outbreak.
The mpox virus has been present in west, central and east Africa for decades, with the first human case identified in 1970. In May 2022, a global mpox outbreak caused by the clade IIb strain of the virus provided the first epidemiologic evidence of community mpox transmission outside of historically affected countries. The Modified Vaccinia Ankara-Bavarian Nordic (MVA-BN, sold as JYNNEOS) vaccine was made available to help contain the outbreak in the United States. The National Institutes of Health’s (NIH) National Institute of Allergy and Infectious Diseases (NIAID) sponsored a study of dose-sparing strategies to extend the limited vaccine supply.
The mid-stage study enrolled 225 adults aged 18 to 50 years in the United States who had not previously been vaccinated against mpox or smallpox. Participants were randomized to receive either the standard Food and Drug Administration-approved MVA-BN regimen, a regimen containing one-fifth of the standard dose, or one with one-tenth of the standard dose. The standard dose was injected under the skin (subcutaneously), while the dose-sparing regimens were injected between layers of the skin (intradermally). Participants in all study arms received two injections 28 days apart and were monitored for safety and immune response.
Two weeks after the second dose (study day 43), participants who received one-fifth of the standard dose had antibody levels equivalent to those of participants receiving the standard MVA-BN regimen, based on predefined criteria. By day 57, participants who received one-fifth of the standard dose had lower antibody levels than those in the standard regimen arm; the clinical significance of this difference is unknown. Participants who received one-tenth of the standard dose had inferior antibody levels at all measurements. The most reported adverse events were mild, local injection-site reactions. Adverse events were similar across all arms of the trial, and no serious adverse events related to the vaccine were reported.
The authors note that because there are no defined correlates of protection against mpox—immune processes confirmed to prevent disease—these findings cannot predict the efficacy of dose-sparing regimens with certainty. Real-world data from the Centers for Disease Control and Prevention and others have shown similar vaccine effectiveness for the dose-sparing regimen given intradermally and the standard regimen given subcutaneously. A study of the standard MVA-BN regimen in adolescents is ongoing and will report findings later this year.
NIH is grateful to the research sites and volunteers who participate in studies to improve the mpox response.
For more information about this study, please visit ClinicalTrials.gov and use the identifier NCT05512949.
Frey et al. Safety and Immunogenicity of Fractional Doses of Modified Vaccinia Ankara-Bavarian Nordic. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Global Congress in Barcelona, Spain. Saturday, April 27, 2024.
